iStock
By Mary Carpenter
“Too much shellfish (oysters, of course) and alcohol (festival life!), and not enough water might have exacerbated this bout,” emailed Europe-based film critic C.M. after waking up on her final morning in New Orleans for the Tennessee Williams Festival with the excruciating pain of gout. What could have helped: avoiding beer, organ meat and tuna; also, drinking coffee and eating cherries!
Only after an ER nurse asked about gout did C.M. remember her diagnosis from years before, but because that had been for a swollen big toe, the classic location for gout, she hadn’t made the connection when intense pain struck her ankle. Also, as she noted, “it’s more common for men to have gout—and I’m not overweight, or a drinker and stopped eating liver.”
Gout is the most common form of inflammatory arthritis and more prevalent now than ever, according to Science Daily, “affecting more than 10 million people in the United States or approximately 5 percent of the adult population.” Still, many Americans think of gout as a disease from a bygone era and one that afflicted “the rich and royal, including American historical figures such as Benjamin Franklin and Thomas Jefferson.”
Postmenopausal women are susceptible to gout because they lack the protective effects of estrogen—although the attacks occur most often in middle-aged and older men. One risk factor for gout is obesity, and its increase in the U.S. population may help explain its rising prevalence. In addition, diuretics that are increasingly prescribed for high blood pressure can lead to dehydration—a major trigger of gout attacks.
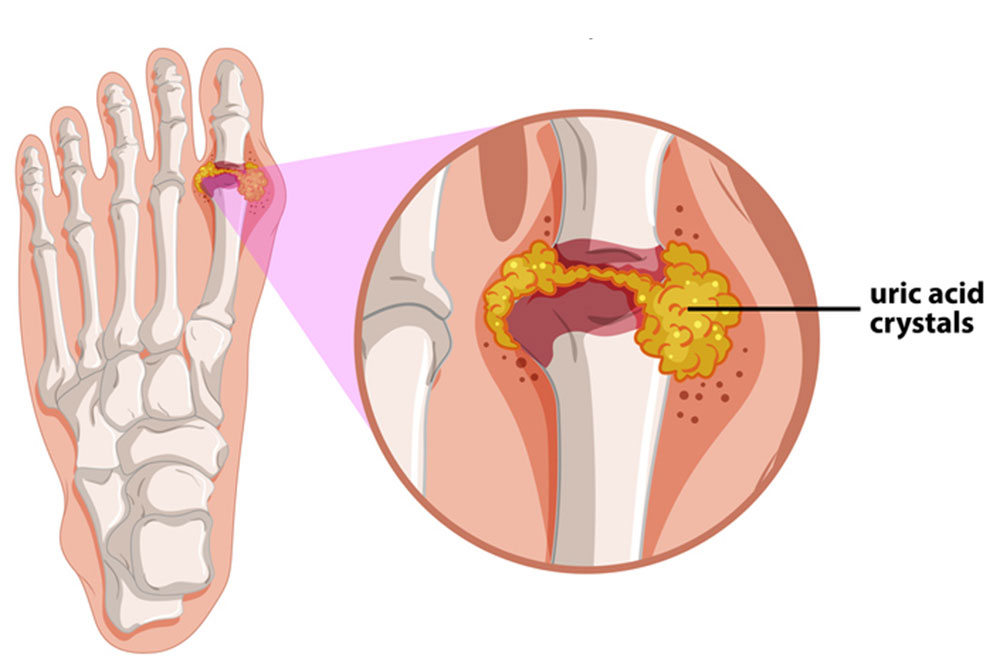
What causes the sudden, rapidly increasing pain that signals a gout flare is the accumulation of uric acid—either when too much uric acid is synthesized in the body or when the removal capacity of the kidney is compromised, according to medical.net. Uric acid results from the breakdown of a chemical called purine —which is present naturally in the body and occurs in high levels in animal proteins, such as pork, red meat, shellfish and oily fish. In addition, alcohol reduces the metabolism of uric acid and can contribute to dehydration.
The buildup of uric acid in the form of urate creates “needle-shaped crystals in and around the joints, usually starting in the foot,” according to Science Daily. Flares occur when the body starts reacting to the deposited crystals, resulting in joint swelling, severe pain and tenderness. Patients suffering from gout for a prolonged period can form nodules of uric acid around the joints, called tophi, and over time gout can progress to “chronic joint damage.”
Besides obesity, risk factors for gout include diabetes, kidney disease, chemotherapy and family history. Of genetic mutations discovered to date, one affects the circulating levels of lubricin, which lubricates and protects joint tissues—and may one day be used as a biomarker for tracing a patient’s risk of developing gout. Another mutation slows the excretion of uric acid, which results in its accumulation in the blood, although high blood levels, called hyperuricemia, are an unreliable indicator of gout.
Diagnosis of gout usually relies on blood and urine testing. The drug allopurinol, used for long-term treatment of gout, can help prevent flares. But for the intense pain of attacks, therapies include glucocorticoids, such as prednisone, and nonsteroidal anti-inflammatory drugs (NSAIDs). Another option is colchicine, a chemical found in many plants—notably wild saffron or autumn crocus—and described for pain and inflammation in the oldest Egyptian medical text, circa 1550 B.C. Investigators who looked into using colchicine for treating Covid found it ineffective.
C.M. had taken allopurinol briefly after her big-toe gout flare, but in New Orleans, NSAIDS quickly alleviated the pain—and she drank more coffee. C.M. wrote, “It was a relatively minor inconvenience…more worrisome than anything else, until I found out what the problem was”— and she hobbled her way through the rest of her trip around the United States.
In my family’s house, gout came up often at the dinner table, because my stepfather who had rheumatoid arthritis also had gout. For someone whose arthritis had caused such severe disability that many of his joints were fused—including his unbending fingers—my stepfather talked about the excruciating pain of gout attacks if anyone suggested one of the foods or drinks believed at the time to trigger flares. Vegetables high in purine, such as asparagus and spinach, were forbidden, although these have since been shown to have no effect on the risk of gout or gout attacks.
We never drank red wine—only white–although “moderate consumption” of either is now permitted. And we never had organ meats or shellfish. But while the current recommendation is to cut back on saturated fats, our several-times-a-week, most-popular, warm-weather meal consisted of summer corn with an enormous steak, grilled black and served very rare— served only with white wine, rather than the better accepted pairing with a full-bodied red.
—Mary Carpenter regularly reports on need-to-know topics in health and medicine.

As always, excellent information.
My husband suffers an occasional flare-up and most of the time we can stop it with loads of water and cherries ( vitamin store has cherry pills if you can’t find the real thing) and of course eliminating the foods for a few days that exacerbate it. Last time he did have to go to urgent care for a cortisone shot which helps a lot. It is so strange that these flares come on so suddenly with no warning. He does take a water pill against my better judgment, which obviously doesn’t help.
Eating even a little too much of the verboten foods can bring on an attack. My husband gets it occasionally, but taking colchicine regularly has made attacks much, much less frequent.
Hi Mary, I think it is important for people who suffer gout first to be sure whether it is gout (usually toe and ankle) or pseudo-gout (often also the knee). A determination can be made by drawing crystals. Doctors may choose different treatment for either. In my case, it was never entirely clear which I had in my ankle, but after allopurinol only reduced the number of attacks, doctors prescribed a daily 0.6mg colchicine instead and I have not suffered an attack for about 15 years.