iStock
By Mary Carpenter
Bruce Willis’s recent diagnosis of frontotemporal dementia or degeneration (FTD) inspired Well-Being editor Mary Carpenter to update her 2018 story—along with recent research that should improve the accuracy of FTD detection, which has been fraught with high rates of false positive diagnoses.
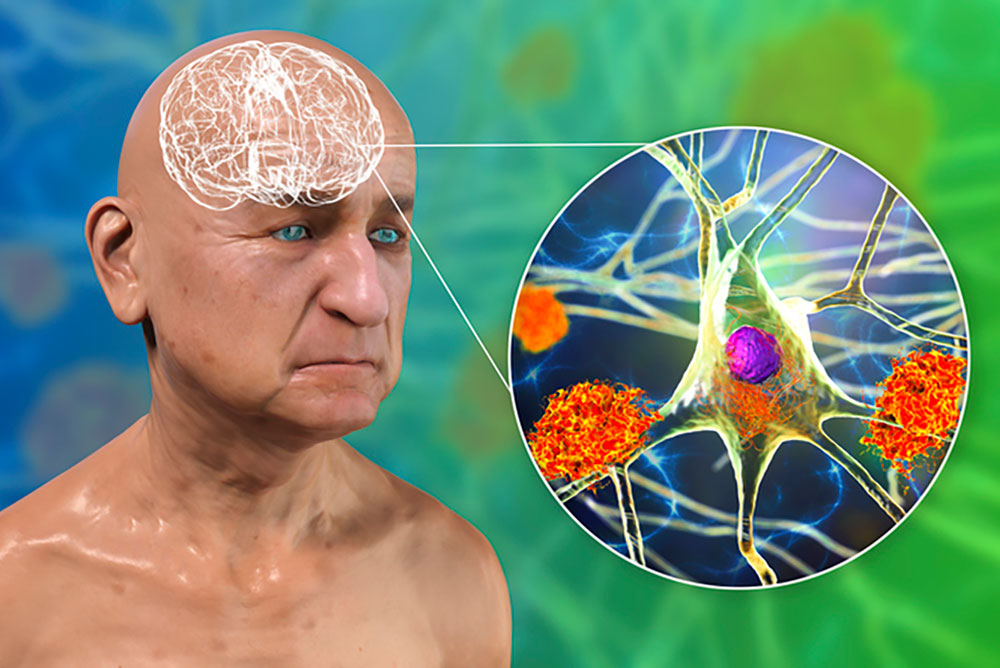
FTD is the most common form of dementia in people under age 65 – beginning at an average age of 58. Explains medical journalist Michele Berman, the behavioral variant of FTD causes changes in personality and behavior—with nerve cell loss “in areas of the brain that control conduct, judgement, empathy, and foresight.”
Diminishing remorse was the almost-imperceptible sign to others after Virginia historian G.E. received a diagnosis of FTD. But for New Jersey filmmaker M.T., it was the room full of unopened boxes after she kept repurchasing the same expensive electronic devices. And M.T.’s most debilitating symptom, “hyperorality,” has caused her to devour inedible objects—sand and dirt, as happens with the condition called pica—along with any food in sight; and to chew on her lips and fingers.
But false positive diagnoses —when in fact FTD is not the reason for symptoms—can cause serious problems. In the case of DC-area nurse P.L., her relatives staged a legal takeover of guardianship based on her erratic behavior, which came in the wake of a tragic loss and was only temporary. Losing financial control, however, meant she was unable to pay for transportation to her work as a nurse and lost several jobs as a result; and her fight to regain independence was long and hard.
Reducing false-positive diagnoses from a high rate of 50% to 69% down to less than 10% was the major accomplishment of a recent multi-center study led by Columbia University neuropsychologist Megan Barker. What makes FTD diagnoses susceptible to error is the inability to examine brain cells directly—and brain imaging is rarely able to detect these problems. False positive diagnoses have occurred most often in younger patients, who usually turned out to be suffering from depression or alcohol abuse.
The seven core features of the condition illuminated by the new study vary depending on where cell degeneration is most prominent —in the frontal and temporal lobes, two of four lobes of the brain that work together. So-called “executive functions”—planning, motivation, inhibition, emotions, and creativity—are mostly controlled by the frontal lobe; while the temporal lobe helps coordinate memory, learning and attention, as well as regulating anxiety levels, appetite and emotion.
Apathy and behavioral disinhibition are the most common and familiar of the seven FTD features, with changes that can at first be small and limited. “Apathy tends to look like the following,” according to the Cleveland Clinic: “loss of motivation, social isolation, decline in self-care and hygiene, compulsive behaviors.”
With disinhibition, sufferers lack self-control and can become rude and self-centered. A dental patient, for example, at the first twinge of pain might slug the dentist—the result of deterioration in the part of the brain that would ordinarily inhibit such a reaction, based on the patient’s knowledge that dental treatment is necessary.
Five features, after apathy and disinhibition, identified by the new study, include irritability/agitation; reduced empathy (sometimes seen as lack of remorse); repetitive behaviors (such as hand clapping); joviality/gregariousness; and appetite changes/orality. A complicating FTD symptom is anosognosia, lack of insight that involves an inability to recognize one’s own symptoms or medical condition, including FTD.
Genetic inheritance plays a role in FTD, with some 30% of cases arising in people with a family history of FTD: having a parent with the mutated gene gives a child a 50% chance of inheriting that gene. In their “update” review, British neurology researchers explain how FTD, because it requires only one copy of a mutated gene from one parent—called an autosomal dominant pattern of inheritance—is a “highly heritable disease.”
Exposing a false positive diagnosis can depend on features of a patient’s condition that are unavailable until long after the first symptoms arise. With an average FTD life expectancy of 7-13 years, for example, an incorrect FTD diagnosis may become evident only after the individual has survived way beyond that time frame. And only a brain autopsy after death can positively identify the neurodegeneration.
Missed cases of FTD—false negatives—on the other hand, most often incorrectly receive the labels of other neurodegenerative diseases, such as Alzheimer’s, Parkinson’s or Huntington’s Disease. And progressive aphasia—the loss of ability to express or understand speech—can be, as in the case of Bruce Willis, an early symptom of FTD; or it can be the correct, final diagnosis.
“Since we announced Bruce’s diagnosis of aphasia in spring 2022, Bruce’s condition has progressed and we now have a more specific diagnosis: frontotemporal dementia (known as FTD),” according to the Willis family statement on the Association for Frontotemporal Degeneration website. “Unfortunately, challenges with communication are just one symptom of the disease Bruce faces.”
I met G.E. on a biking trip, and only once when she returned very late for the next activity were symptoms evident—and her friend told us about the FTD diagnosis. Soon afterwards and before her condition became more challenging, G.E. died in a freak accident. But M.T., a childhood friend, continues to suffer worsening symptoms in a special FTD care center, where she must be carefully watched and often restrained but still manages to harm herself. Friends and relatives of both women are grateful that diagnosis of someone well known like Bruce Willis brings greater awareness of the condition.
—Mary Carpenter regularly reports on need-to-know topics in health and medicine.

Any type of brain dysfunction is devastating, to the patient, but probably more to family and friends, who recognize the loss of the person who was. My mother had dementia, another form of brain dysfunction. My heart breaks for all affected, no matter in which way.
Great job covering this devastating neurological condition, including the difficulty in nailing down an accurate diagnosis. Disseminated information about how socially unacceptable behavior can sometimes be attributed to disease is a good thing… can go a long way in helping generate a wider awareness, and empathy for these conditions.