iStock
By Mary Carpenter
MICRODOSING psychedelic drugs is “akin to walking outside and the sun is suddenly out,” Seattle bartender Erin Royal told the New York Times. Microdosing refers to taking anywhere from 5% to 30% of the full dose, most often of psilocybin or LSD, several times a week, with the most oft-cited goals of enhancing mindfulness and creativity—and often decreasing depression and anxiety. However, two recent, large, controlled studies trace enthusiastic users’ reports to a placebo effect.
Many aspects of the microdosing experience remain poorly understood, such as how the drugs work in the brain and why effects vary so widely among individuals. Also, there’s the question of what is the best dose and formulation for the desired effects —“sub-perceptual,” i.e., not altering perception of reality— for the two most popular microdosed drugs: psilocybin in about 80% of experiences and LSD in the rest.
Taking too little can feel like nothing but too much can make for a challenging or embarrassing day at the office—with no possibility of prediction without experimenting. In fact, only about one-third of microdosers carefully measure the amount; and “most users dose themselves aiming for a …subtle awareness that they’ve taken something” —which can mean closer to half a full dose, writes Dana Smith in the New York Times.
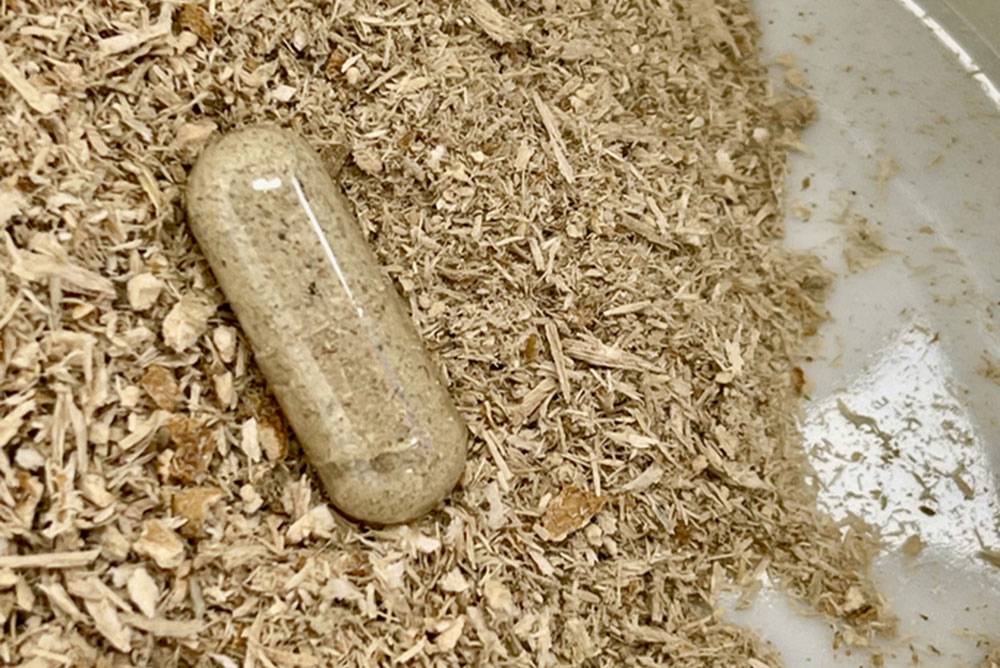
With “stacking,” microdosers combine psilocybin with substances, such as Lion’s Mane mushrooms, chocolate and the B vitamin niacin that helps the body turn food into energy. According to Nature, the goal is “to accentuate salutary effects” by way of either complementary cognitive-enhancing qualities or potential biochemical interactions.
(Another microdosed drug is Lithium, taken at full dose for schizophrenia but in OTC supplements at smaller amounts with the goal of neuroprotection —upping the cognitive vitality that decreases with aging.) Because the supplement formulations of lithium salts also occur in small amounts in drinking water and some foods, people believe these are safer and healthier than prescription medications.
Mental experience-altering chemicals fall into the larger category of biohackers— also called nootropics, racetams, eugeroics—prescription medications taken to boost cognitive function and productivity. The most popular of the “smart drugs” are amphetamines, such as Adderall and modafinil (Provigil), which is prescribed for sleep dysfunction to improve alertness. In a 2008 survey by the journal Nature, one in five readers had taken brain-boosting drugs, half of those using modafinil.
Smart drugs mainly work on the brain via dopamine, which acts as a “reward chemical” but also creates the potential for abuse. And because modafinil improves wakefulness, taking it over time can interfere with sleep—and has given some students the sensation of being neither awake or asleep but trapped in a twilight zone, which risks causing confusion and delirium.
Psychedelics, on the other hand, primarily work on the chemical messenger serotonin that affects mood as well as cognition and memory, Isabelle Grabski writes on a Harvard science blog. According to one hypothesis, psychedelics bind to serotonin receptors in the brain’s cortex responsible for sensory, motor and cognitive functions —leading to hallucinations and other effects.
But the two largest placebo-controlled trials of microdosing—from London and the Netherlands, both published last year—“suggest that the benefits people experience are from the placebo effect,” according to the New York Times. And a third placebo-controlled trial on microdosing LSD at the University of Chicago also found no difference between the LSD and placebo groups.
Study participants, self-selected respondents to a survey, were more likely to be older and live in an urban rather than a suburban area. Potential design flaws in these studies include self-selection as well as the self-sourcing of drugs by participants —making it harder to assess dosage; participants’ prior familiarity with microdosing, which would enable them to guess whether they were taking the drug or the placebo; and self-blinding.
Even when researchers didn’t tell subjects the purpose of the study or what they were taking, the Chicago study found no difference between the LSD and placebo group. And in the London study, 72% correctly guessed when they had taken the drug, leading the authors to conclude: “We could not confirm whether participants followed accurately the self-blinded procedure.”
Changes in brain activity and connectivity seen on scans after single small doses of LSD were similar to what is seen with larger amounts of the drug; and microdoses of psilocybin activated nearly half of the specific type of serotonin receptors acted on by heavier-dose psychedelics. Impact on the brain, however, does not equate with therapeutic value, according to David Erritzoe, clinical director of psychedelic research at Imperial College London. “If you can’t see in a proper trial that it works for…things that people can actually detect and feel and experience in their lives…it’s not that interesting.”
At full doses, psychedelics appear to increase neuroplasticity, which leads to the creation of more and different connections between neurons,” writes Grabski. She describes UC Davis research using the psychedelic DMT, in which microdosed rats continued swimming in a pool with no escape “after the untreated rats had already given up.”
Psilocybin has been as successful as SSRI drugs like Prozac in fighting depression as well as for treating substance abuse, including alcohol, hard drugs and nicotine. For addiction, says NYU psychiatrist Michael Bogenschutz, “The old rule of thumb is that one-third of people get better, one-third stay the same, and one-third get worse.”
But for 15 smokers in an early Johns Hopkins study, psilocybin had a 80% success rate—compared with 35% for those helped by the leading antismoking drug Chantix. The success, according to some experts, is that psilocybin also helps treat smokers’ psychological needs, for example, as a stress release valve. Said one participant at Johns Hopkins, “Now I understand why I smoked…and I don’t need to do that any more.”
“What’s fascinating to me about this whole process [of taking psychedelics] is how many different kinds of experiences people can have, which ultimately help them make these profound changes in their behavior,” said Bogenschutz. For now, however, full-dose psychedelic therapy requires the presence of one or two therapists during the five or so hour-long “trip,” making it too expensive for widespread use or for larger research projects.
A better alternative with similar goals for some people is virtual reality, which has the advantages of increased control of the experience via dose and timing; of not ingesting a chemical; and of creating effects that come from outside the mind with no therapeutic claims. On the other hand, writes Matt Fuchs in the Washington Post, VR “is being used to ease patients into psychedelic-assisted therapy, which overwhelms some people at first.”
Microdosing might be a good way for interested beginners to dip their toes into these experiences—with the hope of enhancing mindfulness and creativity. But uncertainties about dose and timing can make it helpful, even advisable, to have a sympathetic companion on hand, at least in the beginning.
—Mary Carpenter regularly reports on need-to-know topics in health and medicine.
