iStock
By Mary Carpenter
DC-BASED energy consultant A.W. had surgery to remove her gallbladder—after she’d spent 20 years with a diagnosis of irritable bowel syndrome (IBS), which failed to improve despite efforts by many doctors, including five lengthy integrative health work-ups, costing hundreds of thousands of dollars.
“Once IBS is on your chart, no one listens to anything else you say,” A.W. found. She had no pain, but was exhausted and slept all the time; and had only a few foods that she could eat without feeling sick. Then she heard a dinner party guest say he’d had gallbladder surgery for similar-sounding symptoms and had felt great for the first time in years; he recommended his surgeon.
Right away, according to A.W., the surgeon diagnosed gallbladder disease, based on the symptoms and the consistency and smell of her stools—caused by the failure of her digestive system to dissolve fat in her diet. An ultrasound confirmed the diagnosis, and the surgeon removed her gallbladder. Said A.W., “I felt great right away, my fingernails and hair started growing. I had begun to absorb nutrients. And I wasn’t tired any more!”
Because IBS is a “functional diagnosis”—that is, based on self-reporting of hard-to-measure symptoms like pain that have no obvious cause —physicians often pay insufficient attention or fail to look for alternative explanations. IBS is also a diagnosis of exclusion, of eliminating conditions with similar symptoms—including gluten or lactose intolerance; and inflammatory bowel disease (including Crohn’s disease and ulcerative colitis), and gallbladder disease.
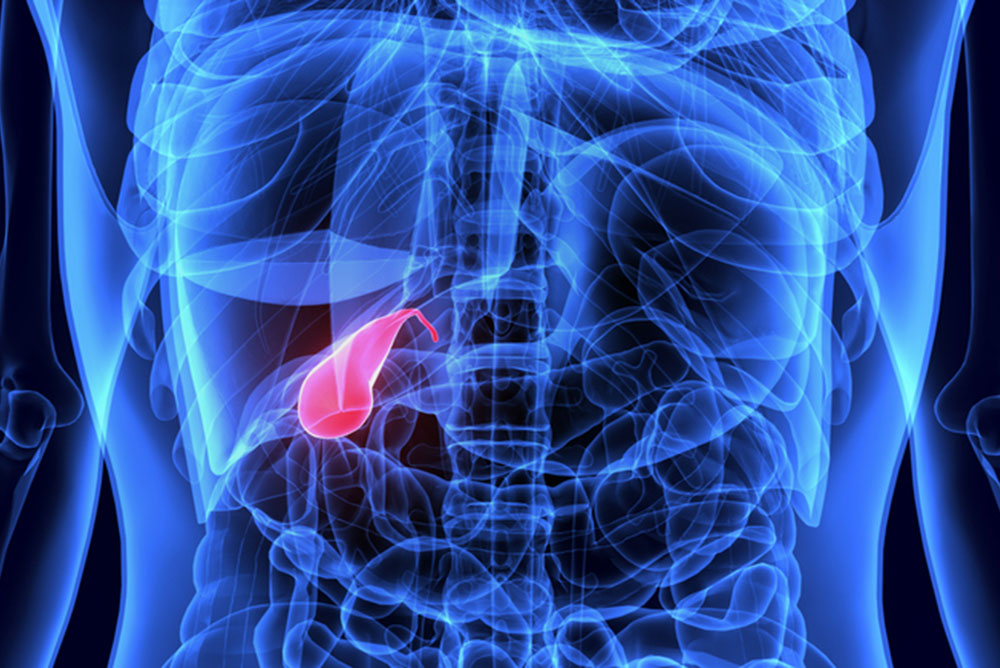
Overlapping symptoms of chronic gallbladder disease and IBS can include nausea, diarrhea and pain. Gallbladder pain arises most often in the upper right section of the abdomen, where the gallbladder is located just below the liver and stores bile produced by the liver. Following meals, bile moves through ducts into the small intestine to help break down fat from food and aid the absorption of nutrients into the bloodstream.
Gallbladder pain, which can also come from just under the breastbone and can radiate to other areas of the chest and upper back, may be severe or mild, though many with gallbladder disease like A.W. have no pain at all. Among other gallbladder-related symptoms, a block or stone in the bile duct can cause yellow-tinted skin or jaundice, lighter-colored stools and dark urine; and an infection may cause chills or unexplained fever. Signs of chronic gallbladder disease can include acid reflux and gas; bloating after meals, particularly those with high-fat content; and chronic diarrhea.
Chronic diarrhea—defined as three or more bowel movements per day for three or more months—when not caused by a condition like Crohn’s or celiac disease, can be a symptom of either gallbladder disease or IBS. In “Habba syndrome,” a dysfunctional gallbladder produces abnormal amounts of bile causing chronic bouts of diarrhea after eating.
IBS, according to the standardized Rome classification system, must include abdominal pain recurring on average at least once a week during the previous three months; and at least two of the following: abdominal pain directly related to bowel movements, and that is associated with a change in stool frequency or in its appearance. To reflect the role of the brain as well as stress in IBS, the Rome system also refers to “changes in how the brain sends and receives” signals from the gut.
Various scans—ultrasound, CT and MRI — can help diagnose gallbladder disease, as can blood tests to check for elevated white blood cells that can indicate infection or inflammation of the pancreas. And functional scans, such as HIDA, employ injections of radioactive material to enable visualization of the gallbladder as it empties over 30 minutes following a meal.
Treatment for excess bile in the gastrointestinal tract can involve changing the constitution of bile acids to decrease the diarrhea, using drugs like Questran that bind to bile acids. And personal activity levels can contribute to the creation of gallstones: one study showed that women who sat for longer than 60 hours a week were more than twice as likely to have surgery to remove gallstones; and an observational study of more than 2,000 people found that a mere two hours of activity per week reduced risk of developing stones by 40%.
Surgery to remove the gallbladder, called cholecystectomy, can have no noticeable effect—although it can take time for the body to adjust to the altered digestion of fat. Temporary effects can include constipation as a result of the surgery; and diarrhea, because bile now flows directly into the intestines as it is produced by the liver. And excess fat or too little fiber in the diet can cause ongoing diarrhea or flatulence,
For a few months after A.W.’s surgery, “food ran right through me,” she said, but as her gut became healthier, nutrient absorption improved and difficulties disappeared. A.W.’s surgeon reported operating on five to ten people a month who had been misdiagnosed for years, some in their 80s, and who recovered to good health quickly afterwards. Many experts agree: when symptoms suggest IBS, gallbladder disease should be considered in many more cases.
Mary Carpenter regularly reports on topical subjects in health and medicine.

Thanks for this great overview of gallbladder disease. A real cautionary tale for all of us. The one person who cares the most about resolving our health problems is the patient him or herself, definitely not the doctor. We really do need to be ever vigilant and proactive.
I think a good message is that we not only need to pay attention to our own bodies and make doctors listen to us, but we also need to make sure we are speaking a language that doctors understand. I’ve recently seen my father, a retired (and elderly) doctor, completely misstate, if not outright ignore, what medical issue he was concerned about to a specialist. And the doctor didn’t know him well enough to start asking the right questions.