iStock
By Mary Carpenter
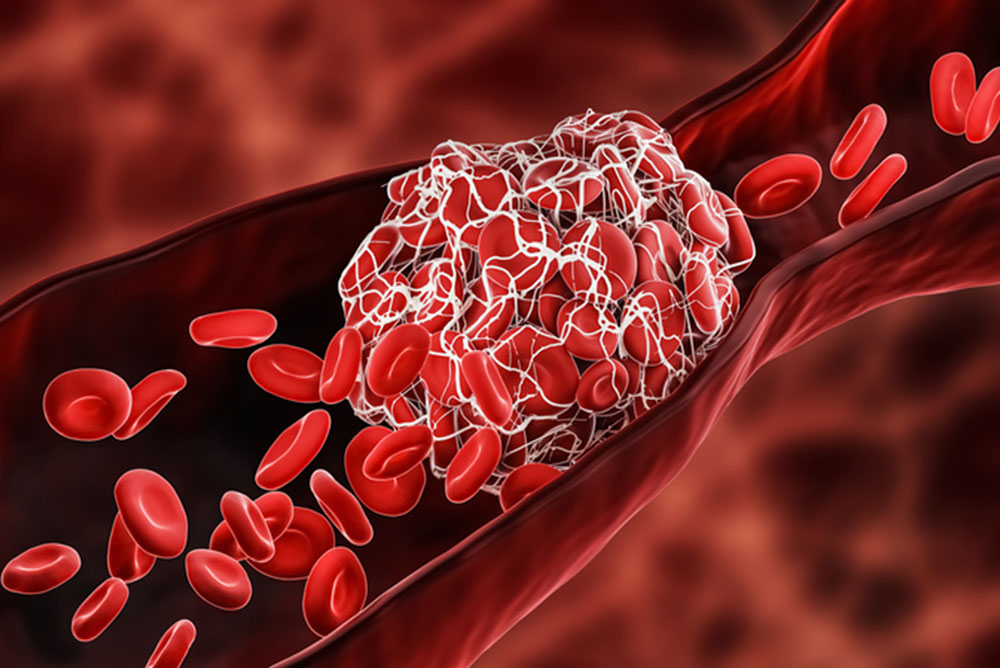
NEW YORK-based science writer S.H. headed for the hospital with back pain that, by the time she arrived, felt “as if someone had taken a baseball bat to my back – though at first it felt as if I had pulled a muscle” in a recent ice-skating fall. The cause: pulmonary embolism (PE), a blood clot that had moved to her lungs.
Dangerous blood clots in the brain and abdomen of those who received Covid-19 vaccines— those made by Johnson & Johnson in the U.S. and elsewhere by AstraZeneca—are unusual, if rare, compared to the more familiar dangers of PE. In the vaccine-induced cases, symptoms include severe headache, abdominal pain, leg pain or shortness of breath within three weeks of vaccination.
After six reported cases of blood clots in the brain—all in women ages 18 to 48, one of whom died—the U.S. suspended use of the J&J vaccine for further study. (Also in the U.S., a seventh woman and a man developed clots after receiving the vaccine during its clinical trials.) Three of the women had “large, dangerous clots” in other parts of the body—not just the brain.
Incidence in the U.S. of dangerous post-vaccination blood clots appears to be at least three times more often than would occur naturally in a similar population of women in that age group, but is still “extremely rare,” according to CDC safety expert Tom Shimabukuro. “Vaccine-induced immune thrombotic thrombocytopenia” or VITT—with the prefix thrombo from the Greek word meaning clump or clot—is the complicated label for these blood clots (the clot is a thrombus, and the formation of clots is thrombosis), accompanied by low levels of platelets (thrombocytes).
While the body’s expected response to the SARS-CoV-2 vaccine involves the creation of antibodies against the coronavirus’s spike protein, in rare cases the vaccine also produces antibodies that bind to platelets—causing them to be “activated and also consumed.”
(As of April 4, the AstraZeneca shot—based like the J&J vaccine on an adenovirus vector —had caused 222 similar cases of VITT throughout Europe, or one in 100,000 of those vaccinated: 169 cases of clots in the brain and 53 cases of abdominal clots; and of 86 cases reviewed, 18 were fatal. As a result, several countries have imposed restrictions on administering the vaccine, either limiting it to people over a certain age, like 50 or 60, or halting its use altogether. )
(When J&J privately requested an informal alliance among vaccine makers to study clotting risks linked to vaccines, AstraZeneca expressed interest but Pfizer and Moderna declined to share relevant risk data for recipients of their vaccines.)
Besides providing time for further investigations into VITT and its causes, the U.S. suspension alerted physicians, not just about the risk, but also about the contraindication in these cases of providing the typical clot treatment that involves the blood-thinner heparin. The reason: When blood clots in vaccine-related cases occur together with low platelet counts, the result is a simultaneous risk of clotting and bleeding — which is paradoxical, because clots are usually the result of abnormally high numbers of platelets clumping together. But the combination is similar to a rare side effect of heparin, which makes the drug a dangerous treatment for vaccine-induced clots. With insufficient information to date about the cause of VITT or why certain individuals are affected, there is no way to predict who might be susceptible.
Blood clots are also a side effect of hormonal birth control—at a much higher rate, of 1 to 5 in 10,000—which led to early downplaying of the vaccine-induced clots. But the comparison is like “apples and cashews,” Michigan ob/gyn Jen Villavicencio told The Washington Post’s The Lily. Clotting spurred by the vaccine sounds more like a syndrome, Villavicencio explained —unlike the single blood clotting episodes that can arise with birth control pills.
In addition, blood clots occur commonly after injury or surgery that damages blood vessels, called deep vein thrombosis (DVT), when platelets flood to the site of injury. While the main role of platelets is coagulation to block excess blood loss, their participation in combating microbial threats and other immune responses has led to a more recent view of them as the “underappreciated orchestrator of the immune system.”
In addition to the birth-control pill connection, clots can occur as side effects of several medications and as a result of illness, or bed rest or prolonged sitting — notably following long airplane trips. Clots occurring in the legs can cause chronic swelling and pain, and cellulitis, a skin infection. DVT rates rise with age, increasing from about 1/1,000 before age 45 to 5 to 6/1,000 by age 80.
The risk increases when a clot travels to the lungs, creating a PE that blocks blood flow. A PE can cause shortness of breath, chest pain and a rapid pulse—but occurs 50% of the time with no symptoms. Unusually, dangerous post-vaccination clots have traveled to the brain and to the abdomen.
In the vaccine-related cases, low platelets developed because the vaccines produced antibodies that mistakenly bound to one of the “clotting factors”—13 different proteins that work with platelets to help blood clot. Hemophilia, a genetically inherited condition, involves the absence or low levels of specific clotting factors—most commonly Factor VIII—which causes sufferers to bleed easily, sometimes spontaneously or internally, and require regular transfusions of plasma to replace the missing proteins.
With VITT and most serious blood clots, treatment is usually successful but recovery can take weeks or longer. After science writer S.H. left the hospital, she had so much trouble breathing that she couldn’t walk a block—which continued for more than a month, along with a no-flying ban.
—Mary Carpenter regularly reports on topical issues in health and medicine.
