iStock
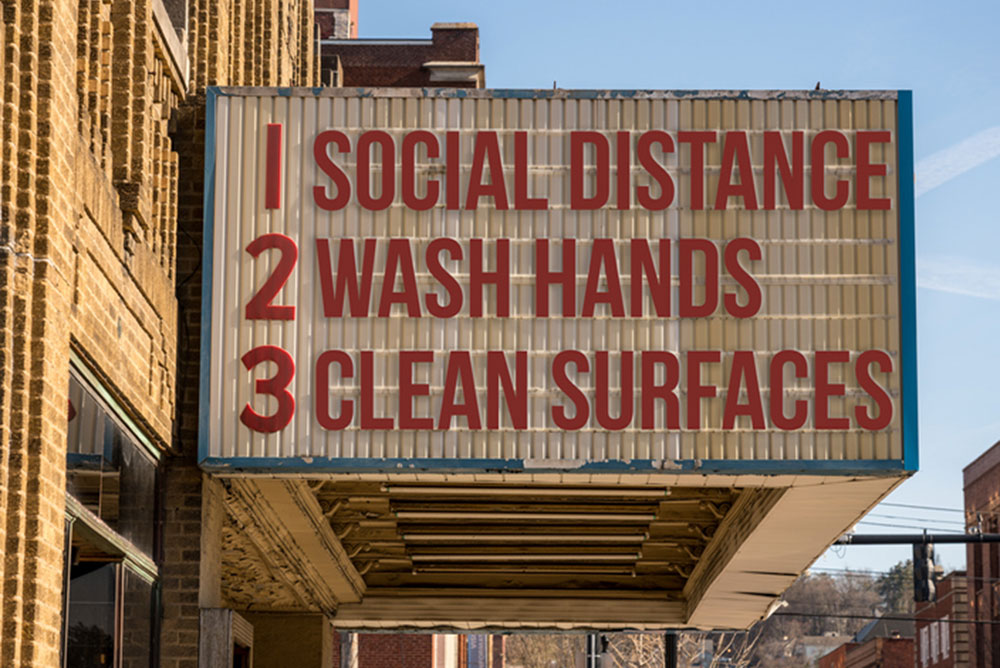
MONTHS OF the coronavirus pandemic have produced valuable information on its modes of transmission and the range of effects on its victims. As localities begin to open up, knowing how to protect yourself and others becomes ever more crucial.
The SARS-CoV-2 virus has three modes of transmission. One is the familiar respiratory droplets, which can carry virus particles or virions about six feet from an infected person but fall quickly to the ground.
Also familiar is transmission via fomites, contaminated surfaces that act as vehicles for the virus. On one cruise ship, forks and knives may have played a major role—with viability lasting up to three days on stainless steel and plastic and about 24 hours on cardboard.
The third mode is aerosols, tiny virion-containing drops that can travel for miles and remain airborne for hours. “Even the smallest breeze will do something,” University of Amsterdam physicist Daniel Bonn told the New York Times.
Aerosols float on air currents—at least as far as barbecue or cigarette smoke, according to Kimberly Prather, aerosol researcher at UC San Diego. Aerosols “can remain infectious in indoor air for hours and be easily inhaled deeply into the lungs.”
Washing hands with soap is the best defense against virus particles picked up from fomites. In all soap—bar or gel—the combination of a fat or oil and an alkali, such as lye, destroys the coronavirus’s lipid membrane, containing the proteins it needs to infect the body. Twenty seconds is the critical amount of time it takes for lathered-up soap to inactivate the virus. (Avoid products that say “soap-free.”)
Masks are the best protection against both droplets and aerosols, Prather contends, noting the success of Asian countries in halting spread of the coronavirus. Taiwan, for example, has had only a few hundred cases and only seven deaths despite never implementing a national lockdown. On average, Asian countries—where people, and especially those who are sick, more commonly wear masks—have counted fewer than 10 deaths per million inhabitants compared with 300 in the US and more than 500 in Britain, Italy and Spain.
Although “silent spreaders,” or asymptomatic carriers, have infected up to 50% of cases, the highest risk occurs when a gathering includes one “superspreader.” Researchers are still investigating what makes some people so infectious.
Dose is the key and depends on three variables: proximity to the infected person, air flow and timing. And the higher the dose for any one person, the more severe the symptoms and the more likely they are to spread infection.
Enclosed spaces with lots of people are the riskiest. Many believe the reason European countries have not seen a spike in cases with their gradual relaxation of restrictions is that, with warmer weather, most large gatherings take place in open outdoor spaces—and most people wear masks.
Besides its transmission modes, SARS-CoV-2 requires many fewer virions than most viruses to establish infection in humans—hundreds of particles compared with thousands for the virulent MERS. And, according to one theory, SARS-CoV-2, unlike most flu viruses, penetrates deep into the lungs, which are designed to move gases in and out of the bloodstream, enabling the virus to make a similar journey.
Also, there is the 10 to 20 times greater affinity of this virus for a receptor (ACE2) found on the outer surfaces of cells throughout the body.
The complicating factor of the ACE2 (angiotensin-converting enzyme 2) receptor: It not only provides a route for the virus into cells, but it can also modulate some of the damage that takes place, according to the New York Times.
For each of the body’s organs, the number of cells with the potential for “ACE-2 expression” affects the likelihood of that organ becoming a reservoir for infection: from 83% of cells in the lungs to 7.5% in the heart and 4% in the kidneys.
“Master of disguise,” one of this virus’s nicknames, refers to the wide variety of symptoms that can appear at different times with different severity—with the added uncertainty of which symptoms are caused by the virus and which by the inflammation created when the body’s immune system overreacts.
For severity of infection, with hydroxychloroquine showing no improved protection to date, researchers are looking elsewhere, for example, to vitamin D, which plays a role in the body’s immune response. Higher levels of vitamin D—which can both bolster the immune system and restrain it from dangerous overreactions—have in some studies led both to better, but also worse, outcomes for Covid-19.
Of every 10 people infected by the virus, about 35% will have no symptoms, and among the rest, symptoms will be mild for about 80%. Although people over 80 are at greatest risk of death from the virus, the presence of other health conditions, or co-morbidities, increases this risk but may vary among different populations.
For heart disease, the risk may be around 9% higher, with diabetes at 7.3% and hypertension at 6.0%. With high blood pressure, which affects almost half of older Americans, abnormalities in blood vessels can impair the ability of oxygen to reach the organs.
In more than 80% of infected individuals, Covid-19 begins with a temperature and a cough; most have a low white blood cell count and nearly all have pneumonia. But infection can also begin with a skin rash that looks like hives or bumps around the toes and heels. And loss of smell and taste occurs in about one-fourth of sufferers.
Infection can also appear first with intestinal problems, possibly a result of the virus traveling directly to the stomach in swallowed saliva. And although stomach acids would normally kill microbes entering the gut, heartburn medications that neutralize the acidic environment might make it more vulnerable to the virus.
For the kidney, degree of injury correlates with worsening respiratory symptoms—either due directly to viral infection or to the inflammatory cytokine storm that causes blood vessels to leak, reducing blood flow and thus oxygen transport to the organs. Blood clots are another serious risk, notably those that lead to stroke, with autopsies of Covid-19 patients showing evidence of small clots in many organs.
Anyone beginning to feel cavalier about SARS-CoV-2 should remember, not just the suffering of older victims, but also the thousands of young sufferers with no co-morbidities but debilitating symptoms that can last months, so called “long-haulers.” DC elementary school teacher Chloe Kaplan, for example, who is in her 30s, with a young child, recently marked Day 78.
—Mary Carpenter
Well-Being Editor Mary Carpenter continues to provide coronavirus updates. To read more of her posts, click here.

Excellent update, thanks so much for keeping on top of this and sharing. I will share with others!
Another comprehensive and helpful article! Just one question. The WHO recently issued a statement that infected but asymptomatic persons rarely spread the virus. Other research sources say that about half of infections are the result of asymptomatic spreaders. Why this disconnect?
WHO walked back that comment earlier today, saying it was a misunderstanding:
https://www.washingtonpost.com/health/2020/06/09/asymptomatic-coronavirus-spread-who/?pwapi_token=eyJ0eXAiOiJKV1QiLCJhbGciOiJIUzI1NiJ9.eyJjb29raWVuYW1lIjoid3BfY3J0aWQiLCJpc3MiOiJDYXJ0YSIsImNvb2tpZXZhbHVlIjoiNTk2YWJmMzVhZGU0ZTIwZWUzNzczOGM3IiwidGFnIjoid3BfbmV3c19hbGVydF9yZXZlcmUiLCJ1cmwiOiJodHRwczovL3d3dy53YXNoaW5ndG9ucG9zdC5jb20vaGVhbHRoLzIwMjAvMDYvMDkvYXN5bXB0b21hdGljLWNvcm9uYXZpcnVzLXNwcmVhZC13aG8vP3dwbWs9MSZ3cGlzcmM9YWxfbmV3c19fYWxlcnQtd29ybGQtLWFsZXJ0LW5hdGlvbmFsJnV0bV9zb3VyY2U9YWxlcnQmdXRtX21lZGl1bT1lbWFpbCZ1dG1fY2FtcGFpZ249d3BfbmV3c19hbGVydF9yZXZlcmUifQ.x6-RRDjxc5V6yFxxM3s_cwmtE0CB1Dog-fHbJPMdBM4&utm_campaign=wp_news_alert_revere&utm_medium=email&utm_source=alert&wpisrc=al_news__alert-world–alert-national&wpmk=1