iStock
By Mary Carpenter
FOUR PATIENTS —diagnosed with different autoimmune diseases and with different symptoms —shared one outstanding variable: their older age, from 59 to 71. Research by NIH Environmental Autoimmunity Group emeritus Frederick Miller found a doubling of autoimmune disease risk markers between 1988-91 and 2011-12—with the greatest rise occurring in two groups: adolescents and older adults. Miller told AARP, “Autoimmune conditions, like most diseases, are diseases of age.”
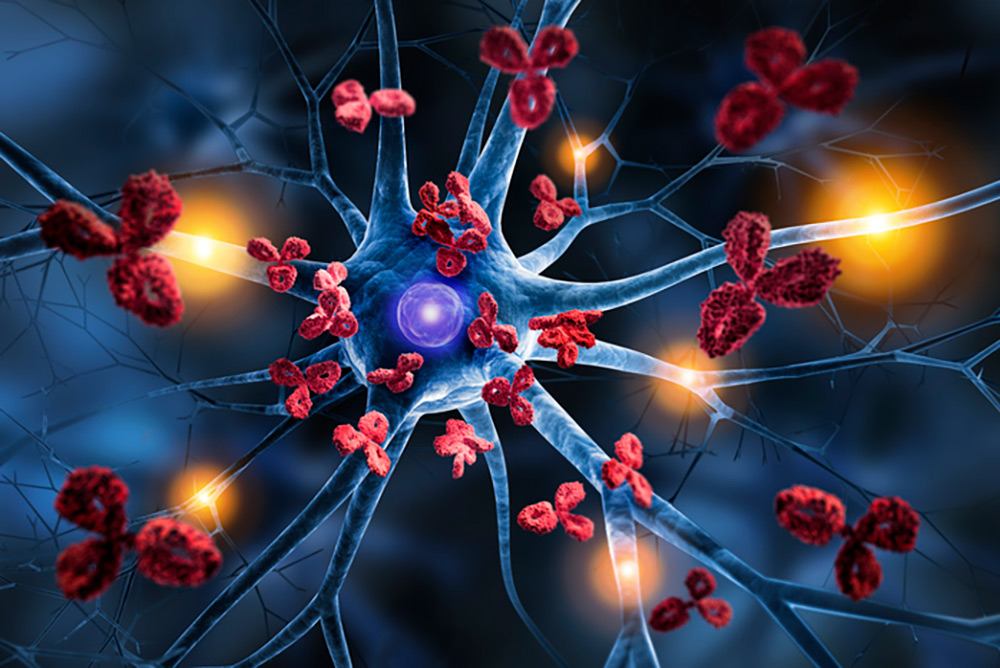
“The explosion in chemicals used—more than 80,000 approved in the past 30 years” is one of Miller’s possible explanations for the recent surge for all age groups in autoimmune diseases. For sufferers, their immune system, which should protect the body from infections and other diseases, instead attacks healthy cells and organs. Among other possible contributors to the surge, according to Miller: changes in diet, including more processed food; more sedentary lifestyles; and “a different pattern of infectious agents, even pre-Covid, with more emerging yearly.”
Normal immune defenses “have essentially gotten confused [by these changes] and set off friendly fire against your own body,” said Timothy Niewold, director of New York University’s Langone Center for Autoimmunity. According to the Langone Center report, cases of autoimmune disease “seem to be rising precipitously, especially among people over age 50 [and are now] 50 percent higher in older adults than they were 25 years ago.”
Women make up about 80% of sufferers around the world of autoimmune diseases, notably Sjogren’s syndrome—which attacks the body’s moisture-producing glands—lupus, MS and most forms of arthritis, except osteoarthritis, according to medical geneticist Karen Orstavit at the University of Oslo. In one long-standing explanation, estrogen levels affect the risk—with many autoimmune diseases in women starting shortly after puberty and often changing during pregnancy.
But a new culprit discovered earlier this year is a molecule called Xist that “triggers a chemical response [in women] that is a hallmark of autoimmune diseases,” according to a Washington Post report calling it “a major clue why 4 of 5 autoimmune patients are women.” But Xist cannot be the sole explanation—because men get autoimmune diseases such as lupus; and Type 1 diabetes has a higher incidence in men—David Karp, rheumatic diseases division chief at UT Southwestern Medical Center, told the Post, “It’s not the only answer, but it’s a very interesting piece of the puzzle.”
Also in the news, semaglutide—the active molecule in the new weight-loss drugs such as Ozempic—appears to help sufferers of “recent-onset Type 1 diabetes…to either eliminate or reduce the need for insulin,” according to the New York Times. Another recent treatment, biologic medications made from living cells, have had results as good or better than the earlier option of stem cell transplantation.
Long Covid shares many of the same “terrible debilitating symptoms”—heart palpitations, crippling fatigue, extreme brain fog, shortness of breath—reported by those with autoimmune diseases, according to a podcast conversation between Ross Douthat and Meghan O’Rourke, writers for the New York Times, the Atlantic and elsewhere. Long Covid symptoms have occurred in up to 30% of those infected by the virus—more often in younger patients, and in some who had mild cases of the disease.
Of the four patients in Miller’s NIH study, a 68-year-old woman who reported insomnia, a tight feeling in her face, and “eyes so dry that no amount of artificial tears could stop the burn,” received a diagnosis of Sjogren’s syndrome. Another, age 59, also had eye symptoms—with her vision in one eye going black for several seconds and afterwards her eyes visibly bulging. The diagnosis was thyroid eye disease, most often seen in patients with one of two autoimmune disorders: Graves’ disease and Hashimoto’s thyroiditis.
Ulcerative colitis, an inflammatory bowel disease, was the diagnosis for the 70-year old NIH patient after what he thought was a stomach bug didn’t go away. And giant cell arteritis (GCA), which affects blood vessels in the head, neck and arms, was the diagnosis in a 77-year old patient, making her arms feel so heavy she struggled to brush her teeth. In a separate report of a Maine potter, age 93, the diagnosis of polymyalgia rheumatica—inflammation causing muscle pain and stiffness—often appears concurrently with GCA, also in people age 50 and older.
Environmental triggers of autoimmunity include viruses and bacteria—but also pollutants and even specific foods that activate the immune system. Gluten is the trigger for Celiac disease; the Epstein-Barr virus for both MS and CFS (chronic fatigue syndrome); and cigarette smoke for rheumatoid arthritis.
The triggers can act by turning on inherited genes that make some individuals more susceptible to developing autoimmunity. Several diseases, such as rheumatoid arthritis, are more prevalent in people with variants of the HLA-B gene—in particular, the HLA-B27 variant, which occurs in 8 of every 100 people, though far fewer than that number have developed related autoimmune disorders.
In my family, with no history of autoimmune disease, two women in their twenties developed autoimmune conditions linked to that variant—ankylosing spondylitis, which can cause spine pain and swelling in the eyes; and lichen sclerosis. Their mother’s testing showed she also had the variant, though by age 65 she had no indication of autoimmune problems.
As happened with the two young women, symptoms of autoimmunity can come and go, and they can be mild. I only discovered long after getting to know two friends that one has Hashimoto’s and the other Sjogren’s syndrome. And genetic links are still emerging: for another friend who has Ehlers Danlos hypermobility, researchers suspect connections to genetic variants that have been found in rare forms of this disease.
The most important lesson came for me, in the same family of my relatives—with the two young women and their mother—when a 70-year-old brother developed debilitating lung issues following a serious winter bout of pneumonia. After months of tests, the most likely diagnosis involved an autoimmune reaction—especially after his symptoms responded to steroid medications, the standard first-line treatment for autoimmune disease.
—Mary Carpenter regularly reports on topical subjects in health and medicine.

Interesting, and concerning. As we all (hopefully) live longer, more health problems emerge. The best we can do is try hard to live as healthy as possible.
The explosion in auto-immune diseases is something I see in my own family with both my young son and daughter-in-law having celiac and lupus, respectively. In the next years, do you think that AI will dramatically advance our understanding of the genetic origins and triggers for many of these disorders?
Interesting and helpful article!