iStock
By Mary Carpenter
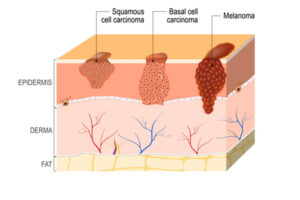
“SQUAMOUS cell carcinoma (SCC) is a life-threatening type of skin cancer,” according to Harvard Health—and not the benign problem that many people think. In the first episode of “New Amsterdam”—a TV series based on the true story of Bellevue physician Eric Manheimer, called Max in the show—the diagnosis came up in ominous tones accompanied by “have you told your wife?”
While most SCCs occur on skin, making them easily visible and often simple to remove in their entirety—those arising inside the body can become more complicated, with a recent case requiring complete jaw reconstruction.
But even when squamous cell carcinomas is on the skin’s surface, diagnosis and treatment are not always straightforward. For former DC area political consultant R.F., his medical team surgically removed SCC lesions—but afterwards shared biopsy slides with two other cancer centers. The team was concerned about the possible presence of spindle cells—specialized cells that are tricky to detect and can indicate the cancer may have penetrated to a deeper level and could be life-threatening.
SCC is the second most common form of human skin cancer—with at least 200,000 to 400,000 new cases of SCC expected each year in the US, according to the American Academy of Dermatology. For comparison, the more worrisome melanoma affects nearly 100,000 Americans a year, with survival rate at five years around 94%—unless it spreads to other areas of the body, notably the lymph nodes.
The most common skin cancer, basal cell carcinoma (BCC), was the diagnosis for First Lady Jill Biden’s skin lesions, removed in early January—and also for lesions removed from Nancy and Ronald Reagan, and George H.W. Bush, according to the Washington Post. Occurring in cells that form the deepest layer of the skin, basal cell carcinoma causes eight of every 10 skin cancers; while it can be aggressive, the lesions rarely metastasize.
“It’s a matter of exposure,” states the mdanderson site, explaining why most skin cancers occur on the head and neck. “Because those are the areas most often left uncovered—so they get the most exposure to UV radiation.” The five-year survival rate for SCC is 99%—although the number drops to about 50% for throat SCC that has metastasized.
For his squamous cell carcinomas, R.F. had Mohs surgery, performed in stages that involve slicing thin layers of skin and examining the cells while the patient waits—and the surgeon continues slicing until cancer cells are no longer present. Also called Mohs micrographic surgery, the procedure includes removal of a margin of cells around the cancerous spot, according to the skin cancer foundation, and allows for “the removal of all cancerous cells for the highest cure rate while sparing healthy tissue and leaving the smallest possible scar.”
Also used to treat First Lady Biden, Mohs is “the most effective technique for treating many BCCs and SCCs,” according to the Skin Cancer Foundation. Physicians often recommend Mohs for skin cancers that are large or aggressive, have edges that are hard to define, occur in certain areas where tissue is thin such as the scalp, or when cancer involves mucous membranes, such as on the lips. For more advanced cases, physicians add radiation or chemotherapy.
Squamous cells line the surface of the skin as well as the interior surfaces of the mouth and stretch down from the oral cavity into the esophagus and lungs—as well as into the cervix, anus and bladder. As surface-lining cells change, tumors can form in the glandular tissue that lines internal organs, such as the lungs, where they are more commonly labeled adenomas and can also become malignant.
UV radiation is the main cause of head-and-neck SCCs on the skin’s surface, which usually begin with suspicious areas that can be tender, raised or higher than the surrounding skin—and don’t improve after several weeks. In some cases, SCC begins with ulcerated sores inside the mouth or a painless lump in the neck that indicates a swollen lymph node. Human papilloma virus may be another cause of SCC in the throat.
For Eric Manheimer, squamous cell carcinoma kept him out of work for six to eight months. In his 2012 book Twelve Patients, Manheimer describes his treatment using “a radiotherapy mask that required him to be bolted down to the table,” according to the New York Post. “It’s a computerized program…the rads are built exactly to your tumor so you can’t move your head at all. It’s a mask molded to your face.” R.F.’s recent journey with squamous cell carcinoma began when he noticed two suspicious spots on his head, which were sore to the touch. During the Mohs surgery, his medical team concluded that they had excised “all traces” of SCC—and follow-up scans over the next five months have been clear. According to R.F., the team “removed any underlying spindle cells— if that’s what they were.”
Recently R.F. learned that his cousin and son had similar skin cancers in locations similar to his. While about 10% of melanomas may be linked to family history, SCC is “generally not inherited, it typically arises from mutations in the body’s cells that occur during an individual’s lifetime…called a somatic mutation,” according to the National Library of Medicine’s MedlinePlus site. But “rarely [SCC] is found in several members of a family [with] inherited disorders that increase the risk of multiple types of cancer.” At last week’s CT scan, R.F. received the good news that he can wait six months before his next visit. His wound continues to require regular care, in part because he chose not to have skin grafts that can help cover the wound but have been linked to increased risk of infection. He urges everyone to get regular dermatologist body scans and pay attention to anything unusual occurring on the skin. Last week, he returned to his weekly swims, wearing “a very tight cap”—and was back on the tennis courts, with lots of sunscreen, of course.
—Mary Carpenter regularly reports on need-to-know topics in health and medicine.

I have seen my dermatologist more in the last 2-3 years than in my whole life. It seems as soon as I have a couple spots (not cancerous) removed, another one pops up. I have never been good about using sunscreen unless I am at the beach and then only on my face (much to my daughter’s chagrin). A good dermatologist is worth his weight in gold. Mine is aging but tells me he won’t retire (what else would he do?).I tried one near where I used to work and he was awful so went back to my local Laurel guy who has been there, well, forever.
Thanks for the very useful information!!