iStock
IN HIGH school, my “big sister” Kate drowned in a swimming pool. I knew Kate had epilepsy—sufferers are almost 20 times more likely to drown (if a seizure occurs while swimming) than the rest of the population.
Epilepsy recently became the first condition for which a CBD-based treatment won FDA approval, though only for two rare, difficult-to-treat forms of the disease. But how CBD alleviates symptoms of epilepsy remains a mystery as do many aspects of the disease itself.
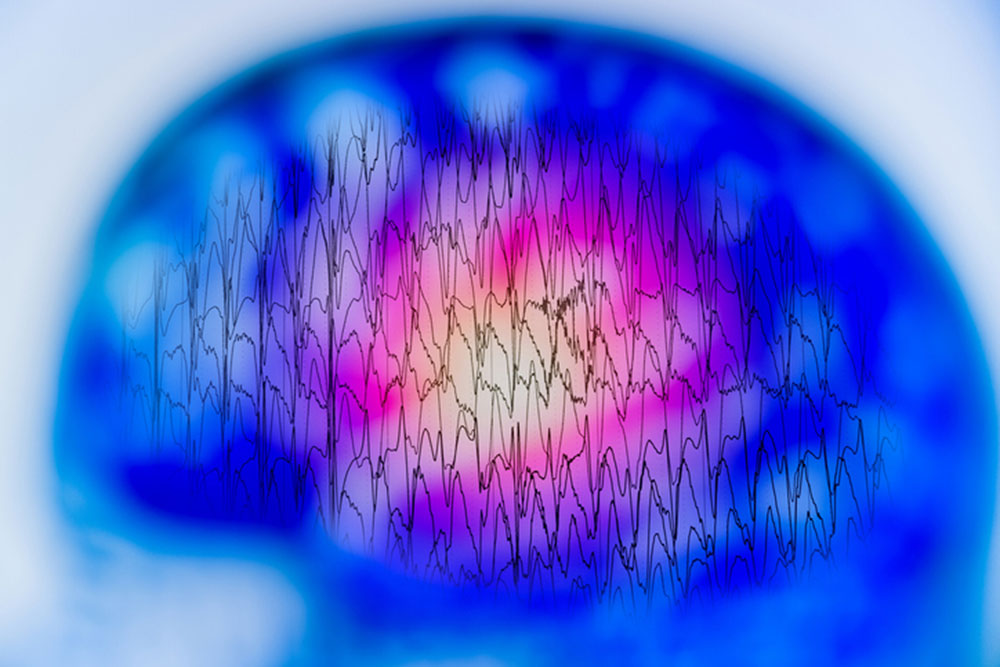
Epilepsy’s definition sounds straightforward: a central nervous system (neurological) disorder in which brain activity becomes abnormal, causing seizures or periods of unusual behavior, sensations and sometimes loss of awareness.
But the disease is not simple. Symptoms can be very different depending on which part of the brain is affected; in about half of sufferers, treatment medications are ineffective or only partially effective, and the cause of their epilepsy is unknown.
In the case of my college friend Pam’s “frontal-lobe epilepsy,” symptoms like grimacing and screaming got her labeled “crazy” by family and friends. “Temporal-lobe epilepsy,” the diagnosis in a recent Washington Post medical mystery, can cause buzzing sensations throughout the body as well as feelings of terror and detachment. Both are ““epilepsy syndromes”, characterized by specific clusters of features involved, such as the part of the brain affected, the cause of the seizures and the age at which they started.
Most anti-seizure drugs work by slowing down excitatory nerve activity in the brain. But debilitating side-effects, such as fatigue, headache, dizziness and vertigo, vomiting and liver damage, can drive sufferers to reject the drugs. When people said about my big sister, “Kate didn’t take her medication,” we heard blame as we did for my friend Pam’s unhinged behavior.
In addition to blaming sufferers, most people have no idea how to react to someone having a seizure, and traditional wisdom is generally wrong. The worst response is putting something in the mouth. Although there’s no risk of sufferers swallowing their tongue, stiffening muscles may tighten during a seizure, causing the person to bite down. If something is in the person’s mouth, they may swallow the object or break their teeth.
Restraining someone having a seizure can make them confused, and in some cases, aggressive. And “rescue breathing” is generally unnecessary and risks injury.
Instead, what’s important is timing the seizure to determine whether medical help is needed. While most seizures last only a few seconds or minutes, some that begin with minor symptoms get worse. If a seizure lasts more than five minutes or causes difficulty breathing, call 911.
Besides timing, reassure the person and keep them safe. Make them comfortable by loosening tight clothes; help them lie down if there’s any risk of falling; and especially if someone is unconscious, turn them on their side with their mouth pointing toward the ground to ease breathing.
For about half of sufferers, epilepsy can be traced to a specific cause such as genetic influence; head trauma; brain conditions such as tumors or stroke; and infectious diseases such as meningitis.
Although symptoms appear throughout the body, the electrical events responsible for epilepsy always occur in the brain. Focal (partial) seizures affect only one area of the brain and often don’t cause loss of consciousness. Generalized seizures, what people used to call “epileptic fits,” involve the whole brain.
Among types of generalized seizures, “absence seizures” may include brief loss of awareness. The other types affect the muscles: tonic (stiffening); atonic (loss of muscle control), clonic (repeated, jerking muscle movements) and myoclonic (brief jerks or twitches of the arms and legs).
The sixth and most dramatic kind, tonic-clonic seizures—previously called “grand mal” —can cause abrupt loss of consciousness, body stiffening and shaking, and sometimes loss of bladder control.
The greatest risk for sufferers of epilepsy is known as SUDEP (sudden unexpected death in epilepsy) that can be linked to no other cause and most often occurs during sleep.
Medications to treat epilepsy, which have increased two-fold over the past ten years, help control seizures for most of the three million Americans with epilepsy—but only when sufferers get the right drug for their particular epilepsy syndrome, which many physicians are still unable to recognize.
Other treatments involve nerve stimulation, using devices that are implanted or placed on the skull. An implantable vagus nerve stimulator has reduced seizures in about a quarter of patients receiving the treatment.
Surgery used to be considered a last resort, but it may also work well in the early stages of temporal-lobe epilepsy. Removing the temporal lobe can stop seizures almost completely in about 60% of sufferers who have the procedure —results that occur in less than 10% of those taking medication alone—and therefore, can be a “true cure” for the disease.
As for CBD, the medication Epidiolex has fewer side effects than traditional epilepsy drugs, although high doses can cause fatigue, diarrhea and liver damage. In one study group, those taking 10 mg had 37% fewer seizures—compared to a 42% reduction in those taking 20 mg—but the lower dose produced fewer side effects and was thus preferable.
Capitalizing on the momentum of Epidiolex approval, researchers are looking into sources of CBD other than the strictly regulated cannabis plants, such as synthetic CBD and CBD produced by “yeast factories” (using a network of enzymes that turn sugar into cannabinoids). These produce a purer, cheaper product and avoid the high water and energy demands that cannabis cultivation makes on the environment.
—Mary Carpenter
Every Tuesday, well-being editor Mary Carpenter reports on health news you can use.

Fascinating. And so interesting that we still don’t know what really causes the disease. Important too to know that there are different kinds of epilepsy…Thank you